Étude clinique sur 31 cas de Tétralogie de Fallot
Objective
To characterize the epidemiological, clinical, and echocardiographic features of dogs and cats with tetralogy of Fallot (TOF) and determine their survival times.
Design
Retrospective case series.
Animals
15 dogs and 16 cats with a diagnosis of TOF as determined via echocardiography.
Procedures
Medical records of dogs and cats were reviewed to extract information on signalment, clinical status at the time of TOF diagnosis, echocardiographic findings, and any outcome data.
Results
The most common canine breeds were Terrier types (n = 7). Most animals (28/31 [90%]) had clinical signs of TOF at the time of diagnosis, including cyanosis (16/31 [52%]). Pulmonic stenosis was characterized by a variable systolic Doppler-derived pressure gradient (median [range], 108 mm Hg [26 to 255 mm Hg]). Most ventral septal defects were large, with a median (range) ratio of the diameter of the ventricular septal defect to that of the aorta of 0.60 (0.18 to 1.15). Median age at cardiac-related death was 23.4 months, with no significant difference between dogs and cats.
Median survival time from TOF diagnosis to cardiac-related death was briefer for animals with no or low-grade heart murmur (3.4 months) than for those with higher-grade heart murmur (16.4 months). After adjustment for age and sex, having a lack of or a low- to mild-grade systolic heart murmur was significantly associated with a briefer survival time.
Conclusions and clinical relevance
With a few exceptions, cardiac-related death occurred predominantly in young adult dogs and cats with TOF, and most animals had severe clinical signs at the time of TOF diagnosis. (J Am Vet Med Assoc 2016;249:xxx-xxx)
Abbreviations
| CI |
Confidence interval |
| ΔP |
Doppler-derived trans-stenotic pressure gradient |
| HR |
Hazard ratio |
| IQR |
Interquartile range |
| LVFWs |
Left ventricular free wall in systole |
| PT:Ao |
Ratio of the diameter of the pulmonary trunk to the diameter of the aorta |
| RVFWs |
Right ventricular free wall in systole |
| VSD |
Ventricular septal defect |
| VSD:Ao |
Ratio of the diameter of the ventricular septal defect to the diameter of the aorta |
Epidemiological, clinical, and echocardiographic features and survival times of dogs and cats with tetralogy of Fallot: 31 cases (2003–2014)
Tetralogy of Fallot has been extensively studied in humans, in whom it is considered the most common congenital cyanotic heart disease, with an incidence of 3 to 5 cases/10,000 live births, accounting for 5% to 10% of all congenital heart diseases.7–9 Several genetic mutations such as those of the genes ZFPM2 and NKX2.5 have contributed to sporadic cases of TOF in humans.4,10
Similarly, TOF is the most common cyanotic heart disease of dogs and cats, accounting for 0.6% to 6.9% of all congenital heart diseases in these 2 species.11–15 The predisposition of Keeshonds to TOF has a suspected genetic basis,16–18 but to the best of the authors’ knowledge, no specific genetic mutation has been identified in dogs.19 Other than the conotruncal malformations reported for Keeshonds,16–18 TOF has been sporadically reported for other canine breeds.20–24 Only a few cases have been reported for cats.11,25–30 Data regarding a series of dogs and cats with TOF are therefore lacking, and survival times of dogs and cats with TOF remain unknown. The purpose of the study reported here was to characterize the epidemiological, clinical, echocardiographic, and Doppler features of dogs and cats with TOF and determine their clinical outcomes and survival times.
Materials and Methods
Medical records review
Paper and electronic medical records were identified of client-owned dogs and cats that had received a conventional (ie, M-mode and 2-D) and standard Doppler echocardiographic examination resulting in a diagnosis of TOF at the Cardiology Unit of Alfort at the National Veterinary School of Alfort, France, and at the Centre Hospitalier Vétérinaire des Cordeliers in Meaux, France, between April 1, 2003, and June 30, 2014. All animals with TOF confirmed by conventional and Doppler echocardiography were included in the study. Animals with equivocal echocardiographic findings were excluded.
Data were obtained from the medical records regarding patient species, breed, age, sex, and body weight. Clinical status at the time of TOF diagnosis, echocardiographic findings (including measurements and presence and types of concomitant congenital heart disease), and any outcome data included in the records were also extracted.
Standard and Doppler echocardiography
Standard 2-D, M-mode, and Doppler echocardiographic examinations were performed while dogs and cats were awake and standing by trained observers at the Cardiology Unit of Alforta and the Centre Hospitalier Vétérinaire des Cordeliers,b as described elsewhere.31,32 Continuous ECG monitoring was provided throughout the examinations. Characteristics of the 4 components of TOF (VSD, overriding aorta, right ventricular outflow tract obstruction, and secondary right ventricular hypertrophy) were assessed via standard parasternal views (Figure 1). Presence of VSD was assessed on right parasternal long-axis 4- or 5-chamber views and by examination of the interventricular septum on right or left longaxis, short-axis, or oblique views.33–35 Transverse views of the heart base, just proximal to the pulmonic valve within the right ventricular outflow tract, were also examined. Color-flow Doppler mode was used to identify and confirm the presence of VSD.33–36 Both color-flow and continuous-wave Doppler modes were used to assess the shunt direction (left-to-right, right-to-left, or bidirectional), as described elsewhere.33–36 Continuouswave Doppler mode was also used to measure the maximal velocity through the defect.
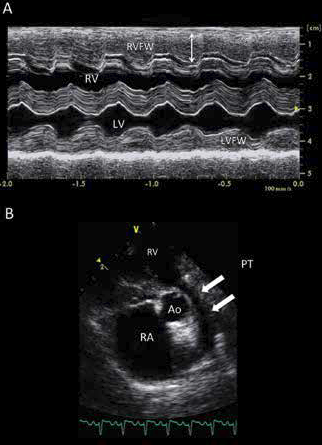
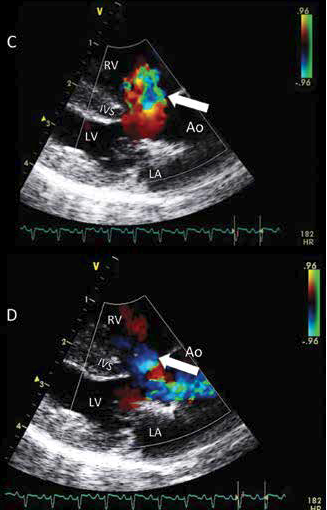
Figure 1—Representative M-mode (A), 2-D (B), and color-flow Doppler (C and D) echocardiographic views of a cat with TOF.
A—The M-mode image reveals severe right ventricular myocardial hypertrophy (double-headed arrow), with a high ratio of right ventricular free wall (RVFW) to left ventricular free wall (LVFW) thickness (1.43).
B—The 2-D left parasternal short-axis view at the level of the aortic valve reveals severe hypoplasia of the pulmonary trunk (arrows), characterized by a PT:Ao of 0.52 without any poststenotic dilatation. Notice also the enlarged right atrial (RA) chamber. This cat was characterized as having a high ΔP value (169 mm Hg) as assessed by continuous wave Doppler mode.
C—A right parasternal 5-chamber Doppler view shows the left-toright component of a bidirectional shunt through a large VSD, located just below the overriding aortic root.
D—Another right parasternal 5-chamber Doppler view shows the right-to-left component of the same bidirectional shunt.
Ao = Aorta. IVS = Interventricular septum. LA = Left atrium. LV = Left ventricle. PT = Pulmonary trunk. RV = Right ventricle.
Maximal size of the defect (ie, VSD diameter) was measured from Doppler color-flow map echocardiograms at the level of the defect through the interventricular septum.33,35 As described elsewhere,35 color-flow Doppler images were analyzed frame by frame to compute the maximum area of the VSD jet signal. The largest color-flow VSD diameter was then measured. Lastly, the transverse aortic diameter was measured along the commissure between the noncoronary and left coronary aortic valve cusps in late diastole by use of a 2-D method, as described elsewhere.31,32 The VSD:Ao was then calculated.
Right parasternal long-axis 5-chamber echocardiographic views were also used to confirm override of the aorta, which was defined as a displacement of the aorta to the right so that it appeared to have a biventricular connection overriding the muscular ventricular septum.2 Right ventricular outflow tract obstruction and obstructive abnormalities of the pulmonic valve and pulmonary trunk (all hereafter referred to as pulmonic stenosis) were diagnosed by means of right and left parasternal short-axis views at the level of the aortic valve. Morphological features of pulmonic stenosis (valvular, subvalvular, and supravalvular obstruction) were assessed from the same views by use of 2-D and color-flow Doppler modes.
Measurements of the diameters of the aorta and pulmonary trunk were obtained by means of a 2-D method and a right parasternal transaortic short-axis view, as described elsewhere.37 Briefly, the end-diastolic diameter of the pulmonary trunk was measured just under the closed pulmonic valve, the aortic diameter was measured on the same view, and the PT:Ao was then calculated. The PT:Ao was considered unremarkable when values in dogs were between 0.80 and 1.15,37 and hypoplasia of the pulmonary trunk was diagnosed when the PT:Ao was < 0.80. A similar cutoff was applied to cats.
Additionally, continuous-wave Doppler mode was used to assess the maximal systolic velocity through the pulmonic stenosis. The modified Bernoulli equation was then applied to calculate the peak ΔP and to grade the severity of pulmonic stenosis. Pulmonic stenosis was considered mild for ΔP values ≤ 50 mm Hg, moderate for ΔP values between 50 and 80 mm Hg, and severe for ΔP values > 80 mm Hg.38
Thicknesses of the RVFWs and LVFWs were measured by means of 2-D-guided M-mode echocardiography on the right parasternal ventricular short-axis view,39 in accordance with the recommendations of the American Society of Echocardiography.40 The ratio of the thickness of the RVFWs to that of the LVFWs was then calculated to assess the severity of right ventricular hypertrophy. Hypertrophy was considered severe when the ratio was ≥ 1.5. Concomitant congenital heart diseases were also recorded.
Follow-up data collection
Follow-up data were collected by a review of the paper and electronic records of only animals with TOF without any other concomitant congenital heart disease. At the time of diagnosis, dogs and cats were classified as clinically or subclinically affected (ie, with or without clinical signs attributed to TOF). Clinical signs for this purpose included exercise intolerance, dyspnea, syncope, and cyanosis. Owners of dogs and cats for which an outcome could not be found in the records at the time the study concluded were contacted by telephone, mail, or email to determine whether their animals were alive (clinically or subclinically affected) or dead (date and cause of death, if known). Dogs and cats for which the outcome could not be obtained at the time the study concluded were considered lost to follow-up and were consequently censored at the time of their last examination on record.
Statistical analysis
Statistical analyses were performed by use of statistical software.c Categorical data are reported as proportions or percentages, and continuous or ordinal data for all variables but survival time are reported as median (range). The Kolmogorov-Smirnov test was used to assess normality of distribution of heart murmur grades and imaging values. Because none of these variables was normally distributed, values were compared between dogs and cats by means of nonparametric Mann-Whitney analysis. Spearman analysis (rs) was used to evaluate correlations between heart murmur grade and ΔP.
Two survival analyses were performed: one for the interval from date of birth to date of cardiac-related death to determine median age at cardiac-related death and the other to assess potential risk factors for cardiacrelated death at the time of diagnosis of TOF. Univariate and multivariate Cox proportional hazard modeling was performed to identify factors associated with survival time. The Kaplan-Meier method was used to estimate median times to cardiac-related death, and these survival times were compared between dogs and cats by use of the log-rank test. Because of the low number of animals, separate multivariate models were developed for each factor hypothesized to be associated with survival time and were systematically adjusted for confounding factors (age and sex). The proportional hazard assumption was checked by including a linear-dependent interaction term, and results (P > 0.13) indicated no deviation from that assumption. Survival times are reported as median (IQR). Values of P < 0.05 were considered significant for all analyses.
Results
Epidemiological features
Fifteen dogs (8 males and 7 females) and 16 cats (11 males and 5 females) with TOF were included in the study, for a total of 31 animals. Twenty-one had received a TOF diagnosis at the Cardiac Unit of Alfort, and 10 had received their diagnosis at the Centre Hospitalier Vétérinaire des Cordeliers.
Dogs were of 9 breeds, with Terrier types predominating (n = 7; 3 Jack Russell Terriers, 2 Maltese Terriers, and 2 Border Terriers), followed by French Bulldog (2), Chihuahua (2), and English Bulldog, Boxer, Cane Corso, and Malamute (1 each).
Median body weight of the dogs was 3 kg (6.6 lb), with a range of 0.5 to 15.2 kg (1.1 to 33.4 lb).
Cats were of 5 breeds, with domestic shorthair predominating (n = 12). Other cat breeds included Persian, Ragdoll, Siamese, and British Blue (1 each).
Median body weight of the cats was 3.2 kg (7.0 lb), with a range of 1.2 to 5.2 kg (2.6 to 11.4 lb).
Overall median (range) age at the time of TOF diagnosis was 7.0 months (1.7 to 54.0 months).
Median (range) age at time of TOF diagnosis for dogs specifically was 3.6 months (1.7 to 49.4 months) and for cats was 9.8 months (2.9 to 54.0 months).
Clinical features
One dog (French Bulldog) and 1 cat (Persian) had concomitant congenital heart disease, consisting for both of an atrial septal defect and subaortic stenosis; values of ΔP were 64 mm Hg and 38 mm Hg, respectively. The remaining 29 (94%) animals had no heart disease other than TOF.
Data obtained from cardiac auscultation at the time of TOF diagnosis were available for 27 (87%) animals (12 dogs and 15 cats). A heart murmur was detected in most (n = 25 [93%]) of these animals. A left systolic basal or midthoracic heart murmur (median grade, 4 [2 to 6]) was detected in 24 (89%) animals, either alone (n = 17 [71%]) or associated with another heart murmur (ie, right systolic midthoracic heart murmur) with a median grade of 4 (2 to 5; n = 7 [29%]), including the dog and cat with concomitant congenital heart disease. One cat had only a systolic right midthoracic heart murmur (grade 5/6).
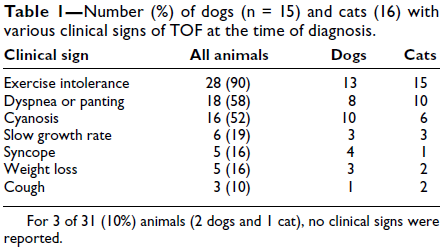
Most animals (28 [90%]) had clinical signs of TOF at the time of diagnosis (Table 1). The most common clinical signs were exercise intolerance, observed in all clinically affected animals, respiratory signs (eg, dyspnea and panting), and cyanosis.
Treatment status at the time of TOF diagnosis was known for all animals. Twenty one (68%; 11 dogs and 10 cats) were not being treated, and 10 (32%; 4 dogs and 6 cats) were receiving 1 or a combination of the following drugs that had been previously prescribed by referring veterinarians: benazepril or enalapril (4 cats and 1 dog), furosemide (1 dog and 2 cats), atenolol (2 dogs), pimobendan (1 cat), acetylsalicylic acid (1 cat), and spironolactone (1 cat).
Echocardiographic features
The location of the pulmonary stenosis was known for 28 of 31 (90%) animals (15 dogs and 13 cats). Subvalvular stenosis was identified in 9 (32%) of these animals (2 dogs and 7 cats), valvular stenosis was identified in 8 (29%) animals (5 dogs and 3 cats), and supravalvular stenosis was identified in 1 (4%) animal (1 cat). Both subvalvular and valvular stenosis were identified in 4 of 28 (14%) animals (3 dogs and 1 cat), and both valvular and supravalvular stenosis were identified in 1 (4%) animal (1 cat). Combined subvalvular, valvular, and supravalvular stenosis was identified in 5 (18%) animals (all dogs).
A description of the pulmonary trunk at the time of TOF diagnosis was available for 28 of 31 (90%) animals (15 dogs and 13 cats). Hypoplasia of the pulmonary trunk was present in 10 (36%) animals (5 dogs and 5 cats). Values for PT:Ao were available for 13 (42%) animals (5 dogs and 8 cats), with a median (range) value of 0.62 (0.31 to 1.22) for dogs and 0.82 (0.52 to 1.40) for cats. The difference between species was not significant (P = 0.51). Three dogs and 4 cats had a PT:Ao < 0.80 (reference range for dogs, 0.80 to 1.1537; reference range for cats unknown).
Values for ΔP at the time of TOF diagnosis were available for 22 of 31 (71%) animals (12 dogs and 10 cats), with median of 108 mm Hg (range, 26 to 255 mm Hg) for all animals. The median value for dogs (106 mm Hg [range, 39 to 255 mm Hg]) did not differ significantly (P = 0.62) from the median value for cats (108 mm Hg [range, 26 to 169 mm Hg]). Pulmonic stenosis was considered mild for 1 dog and 2 cats, moderate for 4 dogs and 2 cats, and severe for 7 dogs and 6 cats. No significant (P = 0.24) correlation was detected between heart murmur grade and ΔP (rs = 0.29).
Data regarding the ratio of the thickness of the RVFWs to that of the LVFWs at the time of TOF diagnosis were available for 17 of 31 (55%) animals with TOF (9 dogs and 8 cats), with a median (range) value of 1.42 (0.89 to 1.94). No significant (P = 0.67) difference in median ratio values was identified between dogs (1.34 [range, 1.25 to 1.94]) and cats (1.42 [range, 0.89 to 1.88]). All 9 dogs and most (6) cats had a ratio > 1, and 7 animals (4 dogs and 3 cats) had severe right ventricular hypertrophy characterized by a ratio > 1.5 (1.67 [range, 1.56 to 1.94]) and (1.79 [range, 1.51 to 1.88]) for dogs and cats, respectively).
A unique perimembranous and membranous VSD was detected in all animals. Data regarding VSD diameter, assessed by color-flow Doppler mode, were available for 26 (84%) animals (12 dogs and 14 cats), with median value of 6.1 mm (range, 1.7 to 15.0 mm). No significant (P = 0.64) difference in median values was identified between dogs (7.7 mm [range, 3.7 to 11.4 mm]) and cats (5.4 mm [range, 1.7 to 15.0 mm]). The median (range) VSD:Ao calculated for 24 of 31 (77%) animals (10 dogs and 14 cats) was 0.60 (0.18 to 1.15), with no significant (P = 0.64) difference between dogs (0.60 [range, 0.35 to 1.02]) and cats (0.58 [range, 0.18 to 1.15]). Twenty one of 24 (88%) animals (9 dogs and 12 cats) had a VSD:Ao > 0.40, and 17 (71%) animals (7 dogs and 10 cats) had a VSD:Ao ≥ 0.50.
The direction of the shunt, assessed by use of combined color-flow and continuous-wave Doppler modes, was available for 29 of 31 (94%) animals (15 dogs and 14 cats). This direction was bidirectional for 15 (52%) of these animals (7 dogs and 8 cats), left-to-right for 7 (24%) animals (3 dogs and 4 cats), and right-to-left for 7 (24%) animals (5 dogs and 2 cats). No animals with left-to-right shunt were cyanotic. All but 1 animal had clinical signs at the time of diagnosis, including exercise intolerance (2 dogs and 4 cats), dyspnea or panting (1 dog and 2 cats), weight loss (1 dog), and slow growth rate (1 dog and 1 cat).
Cardiac events and survival time
Two animals with TOF (1 French Bulldog and 1 Persian cat) were excluded from subsequent statistical analyses because of other concomitant congenital heart diseases (subaortic stenosis and atrial septal defect for each). The dog was euthanized at 75.4 months of age because of right-sided congestive heart failure. The cat died suddenly at 12 months of age.
Of the remaining 29 animals (14 dogs and 15 cats), 25 received a follow-up examination after TOF diagnosis. Eighteen (72%) of these animals remained untreated, and treatment of the other 7 (28%) animals remained unchanged. Hydroxyurea was occasionally prescribed by the referring veterinarian for 1 dog, and phlebotomy in response to Hct values was performed for another dog.
For all dogs that died during the study period (n = 9), death was related to cardiac events at between 3.5 and 92.9 months of age. Cause or nature of death was spontaneous (associated with worsening of clinical signs such as exercise intolerance, respiratory distress, and inability to remain in the standing position) for 4 dogs, euthanasia for 2 dogs, sudden for 2 dogs, and pulmonary embolism for 1 dog. Death was related to cardiac events at between 6.2 and 83.5 months of age for 10 of the 11 cats that died during the study period. Cause or nature of death was spontaneous (associated with exercise intolerance, tachypnea with marked cyanosis) for 4 cats, euthanasia for 3 cats, and sudden for 3 cats. The remaining cat died at the age of 65 months because of infectious peritonitis.
Kaplan-Meier curves of intervals between birth and cardiac-related death revealed that the median age at death for the 29 animals was 23.4 months, with no significant (P = 0.30) difference between dogs (13.0 months) and cats (23.4 months; Figure 2). Median survival time after TOF diagnosis was 14.5 months (IQR, 4.4 to 29.5 months), with no significant (P = 0.73) difference between dogs (11.1 months) and cats (15.3 months).
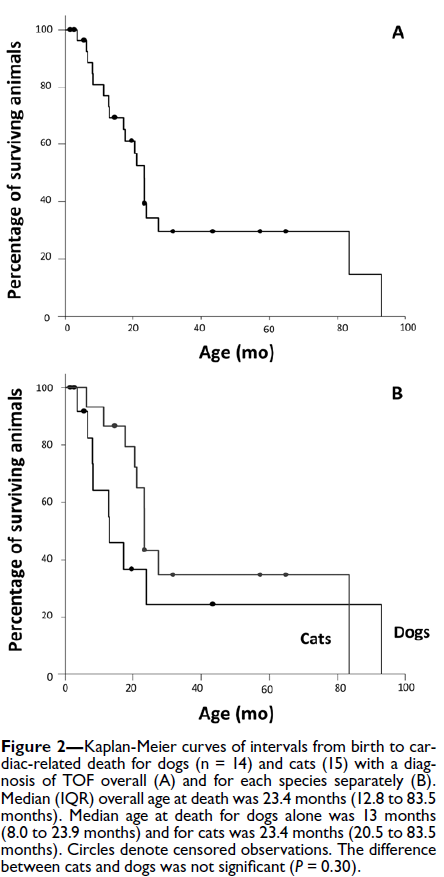
Univariate analysis revealed that animals without any heart murmur or with a low- to mild-grade systolic heart murmur survived for a median (IQR) time of 3.4 months (2.9 to 4.4 months) after TOF diagnosis, compared with 16.4 months (10.6 to 29.5 months) for animals with a higher-grade heart murmur (P < 0.01; Figure 3). The crude HR for this comparison was 14.2 (95% CI, 2.6 to 76.7). Similarly, animals with severe right ventricular hypertrophy had a significantly (P = 0.02) briefer survival time after TOF diagnosis than did animals without this disease characteristic (crude HR, 7.3; 95% CI, 1.4 to 36.6). Males (crude HR, 2.6; 95% CI, 0.9 to 7.6; P = 0.08) as well as animals with cyanosis (crude HR, 2.5; 95% CI, 0.9 to 7.2; P = 0.09) had a briefer survival time after TOF diagnosis than did females or animals without cyanosis; however, these differences were not significant. No significant (P > 0.21) association with survival time was identified for species (dog vs cat), syncope, slow growth rate, presence of severe stenosis, VSD:Ao ≥ 0.5, pulmonary hypoplasia, or shunt direction.
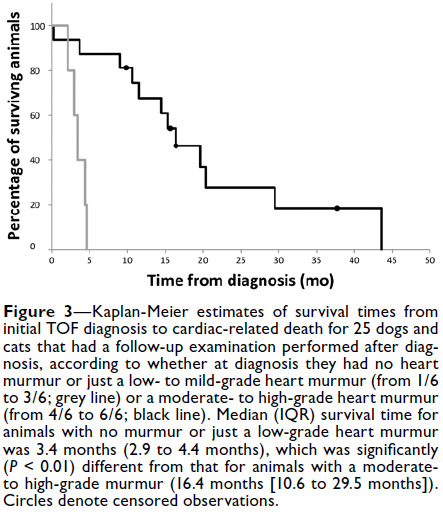
After adjustment for age and sex, lack of or lowto mild-grade systolic heart murmur remained significantly (P < 0.01) associated with a briefer survival time (adjusted HR, 13.8; 95% CI, 2.4 to 80.0) after TOF diagnosis, but the association between severe right ventricular hypertrophy and survival time (adjusted HR, 4.4; 95% CI, 0.8 to 23.5) was no longer significant (P = 0.08).