Extraction of urethral calculi by transabdominal
cystoscopy and urethroscopy in nine dogs
Objectives
To describe a minimally invasive technique for treating urethral obstructions in male dogs and to review the postoperative results.
Methods
All dogs (n=9) had urethral obstruction due to calculi. Obstructions were verified by radiographic and ultrasonographic examinations. Dogs with impaired kidney function were not included in the study. A 5-mm diameter trocar and cannula were placed in the ventral midline, 2 cm cranial to the umbilicus, allowing placement of a 10-mm diameter cannula under visual guidance, adjacent to the apex of the bladder. The bladder was then partially exteriorised and sutured to the skin. A 5-mm diameter cystoscopy sheath was introduced into the bladder lumen and advanced into the urethra.
Continuous retrograde flushing was used to dislodge the calculi from the site of obstruction and collect them upstream.
Results
The nine dogs were followed up for a minimum of 6 months. No major postoperative complications were identified. One dog exhibited transient macroscopic haematuria (for 3 weeks postoperatively). All urethral calculi were removed in the nine dogs. No recurrence was found during the follow-up period.
Clinical significance
A minimally invasive approach is used to treat urethral obstructions resulting from calculi in the male dogs.
Introduction
Urethral migration of cystic calculi is a common cause of urinary obstruction in dogs especially males (Franti and others 1999).
Small breeds are most commonly affected (Adams and others 2008), which is a limiting factor for endoscopic exploration.
The most commonly reported site of obstruction is immediately proximal to the os penis, which may be due to the relatively narrow urethral diameter in this region (Osborne and others 1999). Non-surgical techniques of urethral calculus removal using lithotripsy and basket retrieval have been described. Urethral perforation and stricture are occasionally described complications associated with these techniques, although they can also result simply from the presence of a urethral calculus (Osborne
and others 1999).
The nature of the calculus also plays a role: based on its composition, the surface smoothness varies (Franti and others 1999). Calculi with an irregular surface can abrade the mucosal surface and increase the risk of iatrogenic urethral injury during retrograde hydropulsion attempts.
The technique of choice for relieving urethral obstruction, due to calculi, is to perform hydropulsion, using a urinary catheter suitable for the diameter of the urethra: After emptying the bladder by cystocentesis, the catheter is advanced to the calculus and then flushed with saline to raise intraluminal pressure and so expand the urethra and disengage the urethral mucosa from the calculus. Any temptation to advance the catheter, during flushing, should be resisted as it risks iatrogenic urethral trauma (Osborne and others 1999).
Flushing is essential, but is limited by the bladder’s filling capacity, so repeated cystocentesis may be required during flushing of the urethra. An excessive cystic pressure will also predispose to ureteral reflux and to renal pelvis dilatation.
The minimally invasive surgical technique, described in this article, offers a method of relieving urethral obstruction with a lower risk of urethral, bladder or ureteral injury.
Materials and methods
Dogs included in the study were presented to the Hospitalier Vétérinaire des Cordeliers with partial or complete penile urethral obstruction due to urinary calculi lodged at a site proximal to the os penis. They were treated using transabdominal urethroscopy to relieve the obstruction.
Preoperative investigation included a haematological and serum biochemical analysis (urea, creatinine, glucose, alanine aminotransferase, alkaline phosphatase, total protein and phosphorus), an ultrasonographic examination of the urethra, bladder and the kidneys and a radiographic examination centred on the os penis. A urinary sample was taken from each dog, by cystocentesis, in an aseptic manner, to perform bacterial culture, urine chemistry and sediment analysis. When bladder distension appeared subjectively uncomfortable for a dog, cystocentesis was also employed to empty the bladder. As part of the preoperative stabilisation protocol, attempts were made to reestablish urine flow in all dogs. Gentle advancement of a urethral catheter was attempted or, if urethral calculi prevented its passage, cystocentesis was performed.
The laparoscopic technique, described in this report, was used to retrieve lower urinary tract calculi in all dogs which were presented. The cases (n=4) where a urethral calculus was returned to the bladder, during the course of initial urethral catheter placement, underwent the same laparoscopic procedure to retrieve calculi from the bladder, but were not included in this report which focuses on the laparoscopic relief of urethral obstruction due to urinary calculi. The authors opted to include only those dogs that had no biochemical evidence of renal failure upon admission, in this report, in order to obtain as homogenous a study group as possible. Surgery was carried out under the same anaesthetic. Nine dogs met these criteria over the period from September 1, 2004 to December 31, 2007. The surgical technique used was the same in all nine cases.
Surgical technique
The dogs received preoperative intravenous injections of 15 mg/kg cephalexin monohydrate (Rilexine; Virbac) and 4 mg/kg carprofen (Rimadyl; Pfizer), respectively. General anaesthesia was induced using a combination of intravenous 0-2 mg/kg midazolam (Midazolam; Aguettant), 0-2 mg/kg morphine hydrochloride (morphine; Lavoisier) and propofol (Rapinovet; Shering Plough) dosed to effect to allow endotracheal intubation. Inhalational anaesthesia was maintained using a combination of isoflurane (Forène; Baxter) and oxygen. The abdomen was prepared for surgery in a standard fashion; the dog was placed on the surgery table in the Trendelenburg position (dorsal recumbency, head down tilt) with the surgeon standing by the head of the dog.
A 5-mm diameter trocar and cannula (Karl Storz, Germany – 30160 V) were placed through a 5-mm midline incision of the skin, the linea alba and peritoneum, 2 cm cranial to the umbilicus. The trocar was removed and an insufflator attached to the cannula stopcock. The abdomen was insufflated to a pressure of 12 mmHg using a CO2 insufflator (DMV Medizintechnik, Germany), to establish CO2 pneumoperitoneum. A 2-7-mm diameter 0° telescope (Optomed, France) was introduced through the cannula. The bladder apex was identified, using the telescope, and the surgeon then indented the abdominal wall, with a finger, to locate the site adjacent to the bladder apex. A 10-mm diameter trocar and cannula (Xion, Germany) were then introduced immediately adjacent to the bladder apex. The trocar was removed and a Babcock grasping forceps (Aesculap PO959R) was introduced through the 10-mm cannula to grasp the bladder apex so as to bring it into contact with the abdominal wall (Fig 1).
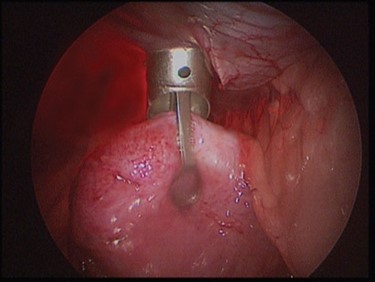
Fig 1 – Forceps inserted in the operating canal to grasp the apex of the bladder
The abdomen was deflated and all laparoscopic instrumentation was removed from the peritoneal cavity; the bladder was partially exteriorised through the abdominal incision of the 10-mm cannula. A 2-0 gauge poliglecaprone 25 suture material (Monocryl; Ethicon) was used, in a simple continuous pattern, to appose the bladder wall to the skin incision edges and so create a seal between the skin and the bladder. A stab incision of the bladder wall was made, using a No. 11 scalpel blade, and then a suction probe was inserted into the bladder lumen to empty it of urine and any sediment. A 5-mm diameter cystoscopy sheath (Optomed, France) was then placed through the bladder incision (Fig 2) and suction tubing was connected to one of the stopcocks of the sheath. The sheath contained two channels: one channel to accommodate a 2-7-mm diameter 0° telescope (Optomed, France) and the other an operating channel through which fine forceps could be introduced.

Fig 2 – Optical device with an operating canal is placed through a small opening in the bladder
A urethral catheter, of the largest possible diameter (10 F, 3-3 mm Arnolds), was inserted into the distal urethra until it touched the calculus; it was then connected to a uropump (Uromat; Karl Storz, Germany) to deliver a continuous flow of lactated Ringers solution, heated to 38°C, at a pressure no greater than
200 mmHg. The telescope and cystoscopic sheath were then advanced together, under visual guidance, past the trigone and into the proximal urethra and then as far as possible along the pelvic urethra until the urethra began to curve at the perineum.
The diameter of the cystoscopic sheath was just less than the urethral luminal diameter, so that the flushing fluid, introduced via the urethral catheter, exited almost entirely through the stopcock of the sheath. This technique helped to isolate a very short section of the urethra between the calculus and the cystoscopic sheath, providing an effective means of dilating the urethra adjacent to the calculus. When the sheath stopcock was closed, this section of urethra was rapidly dilated, disengaging the urethral wall from the calculus. Opening the stopcock then reestablished fluid flow, carrying the calculus proximally towards the sheath.
This manoeuvre was repeated as necessary until the calculus was displaced back into the pelvic urethra whereupon a grasping forceps (Optomed, France – 50 PE051802) was introduced via the operating channel of the sheath, to grasp and extract the calculus (Fig 3).

Fig 3 – A grasping forceps is introduced in the instrument to grasp and extract the calculus
This procedure was repeated if several urethral calculi were found; the bladder was then inspected to identify further calculi which were then retrieved either by suction through the stopcock of the sheath, if they were small, or with the grasping forceps. One or more biopsies of the bladder lining were obtained, from areas with gross lesions, using a biopsy forceps (Optomed, France – PE 051800) which was inserted into the operating channel of the sheath.
The bladder wall stab incision was repaired using two simple interrupted sutures of 3-0 poliglecaprone 25 (Monocryl; Ethicon). The simple continuous suture sealing the bladder wall to the skin was removed and the bladder returned to the abdomen. The linea alba incision and skin incision were closed in a simple interrupted pattern using 2-0 polyglactin 910 (Vicryl; Ethicon) and 3-0 polyamide suture material (Ethilon; Ethicon), respectively.
The retrieval of all the calculi was confirmed by radiographic and abdominal ultrasonographic examinations immediately after the procedure.
Results
Two dogs had already undergone surgery. Both dogs underwent standard ventral midline coeliotomy and cystotomy to retrieve cystic calculi, 2 months and 2 years, respectively, before they were presented to our facility.
Breeds represented included three Yorkshire terriers, two poodles, one Lhasa apso, one cocker spaniel, one French bulldog and one English bulldog. The mean age was 7-9 years (range 2 to 12 years). The mean weight was 11 kg (2-5 to 25-2 kg). One dog was neutered.
Clinical findings
Clinical signs included stranguria (n=1), haematuria (n=1) and pollakiuria (n=1). The mean duration of these clinical signs was 2 days (range 1 hour to 7 days). Some dogs had abdominal pain (n=8), lack of appetite (n=2) and lethargy (n=2). Seven dogs had partial obstruction: their ability to urinate was maintained but the rate of urine flow, during micturition, was severely reduced.
Two dogs were considered to have total urethral obstruction, both for at least 6 hours before presentation, based on their observed posturing to urinate with a complete absence of urine flow.
Haematological analysis demonstrated no major anomalies apart from one dog that exhibited a moderate leukocytosis (19,900 WBC/ml). One dog had an increased alanine aminotransferase value (586 UI/l), the reason was unknown. The cytological examinations carried out on the urine samples obtained by cystocentesis showed haematuria in all cases.
The radiographic examinations showed, in seven dogs, the presence of radio-opacities immediately caudal to the os penis; these were interpreted as urethral calculi. In two cases, multiple
calculi were counted (n=2 and n=3) and in the five other cases, only one radio-opacity was identified. In six cases, the radiographic examination also demonstrated the presence of radioopacities in the bladder.
The ultrasonographic examinations showed no anomalies external to the urinary system. Images compatible with the presence of cystic calculi were obtained in all dogs and all bladders demonstrated an ultrasonographically thickened mucosa, compatible with cystitis. The abdominal urethra and the perineal urethra were visualised over the greatest possible length. No structural injury was identified. Urethral dilatation was subjectively considered as severe, based on ultrasonographic examination, in the two dogs with complete urethral obstruction. No ultrasonographic abnormalities of the kidneys or ureters were identified.
The surgical time ranged from 35 to 95 minutes (mean 55 minutes, median 45 minutes) due to variation in the number and size of the calculi. Smaller urethral calculi (<1 mm diameter) could be retrieved by suction alone, whereas large calculi (>1 cm diameter) often required fragmentation before retrieval, by introducing a 4-mm Kerrison rongeur (Medlane) parallel to the cystoscopic sheath. This additional intervention, with the limitations of minimally invasive surgery, was time-consuming. Most of the surgical time was employed in emptying the bladder of calculi; the disengagement and retrieval of the urethral calculi never took more than 5 minutes.
No dog suffered any postoperative infection. In all cases, the number of calculi extracted from the urethra was greater than that indicated by preoperative imaging (range 2 to 7, mean 3-7).
The results of the histopathological examinations demonstrated the existence of a non-specific chronic cystitis in all dogs.
No bacteria were cultured from any of the urine samples. Calculi analysis results were 100% oxalate (n=5), 90% oxalates/10% magnesium ammonium phosphate (n=2), 100% magnesium ammonium phosphate (n=1) and 100% ammonium urate (n=1).
Postoperative management
No major complications were identified and all dogs were discharged within 24 hours of the surgery. Pain was monitored using the modified Glasgow pain scale (Holton and others 2001). Dogs were assessed every hour postoperatively. Morphine hydrochloride, at a dose rate of 0-2 mg/kg, was given iv when the pain score exceeded 3. No dog required opioid-based analgesia for more than 6 hours postoperatively.
Dogs were discharged with courses of 4 mg/kg carprofen (Rimadyl; Pfizer) once daily for 3 days and 15 mg/kg cephalexin monohydrate (Rilexine; Virbac) twice daily for 5 days after which a negative bacterial urine culture was obtained in all dogs.
Dogs underwent clinical examination at 5 days, 15 days and 3 months postoperatively during which the owners were questioned regarding any clinical signs. All the dogs displayed transient postoperative haematuria (duration range 2 to 20 days, median 3 days).
One dog exhibited severe stranguria the day after it was discharged from hospital. The dog was re-presented to our facility with a full bladder and there was an initial concern of further calculus obstruction. No obstruction was identified, a urethral catheter was passed without any resistance and the bladder emptied. No additional intervention, investigation or treatment was performed and no further stranguria occurred. The episode was attributed to a traumatic urethritis related to the surgical procedure.
The nine dogs were followed up for a minimum period of 6 months (range 6 to 30 months, median time 12 months); no episodes of urinary dysfunction or recurrence of urethral obstruction were identified.